Can the hormonal coil cause acne? And what can you do about it?

Contraception can be a minefield, with women, unfortunately, used to settling for an option that comes with some sort of negative side effect. And if you're on the hormonal coil, you might be wondering if your breakouts are related or not, fed up with having to put up with it.
While you may have been told the hormones are mainly localised (to the womb) and therefore make it less likely for you to experience unwelcome symptoms of other contraceptives (like anxiety and low mood from the pill), what do you know about how it can affect acne?
Here we consult Dr Alexandra Paolino, consultant dermatologist at the Cadogan Clinic, and Dr Babak Ashrafi of Superdrug Online Doctor about whether the hormonal coil could be responsible for your spots, how long your skin will take to improve if you get it removed, and what non-acne inducing alternatives there are. Plus whether natural alternatives are reliable or not.
Can the hormonal coil trigger acne?
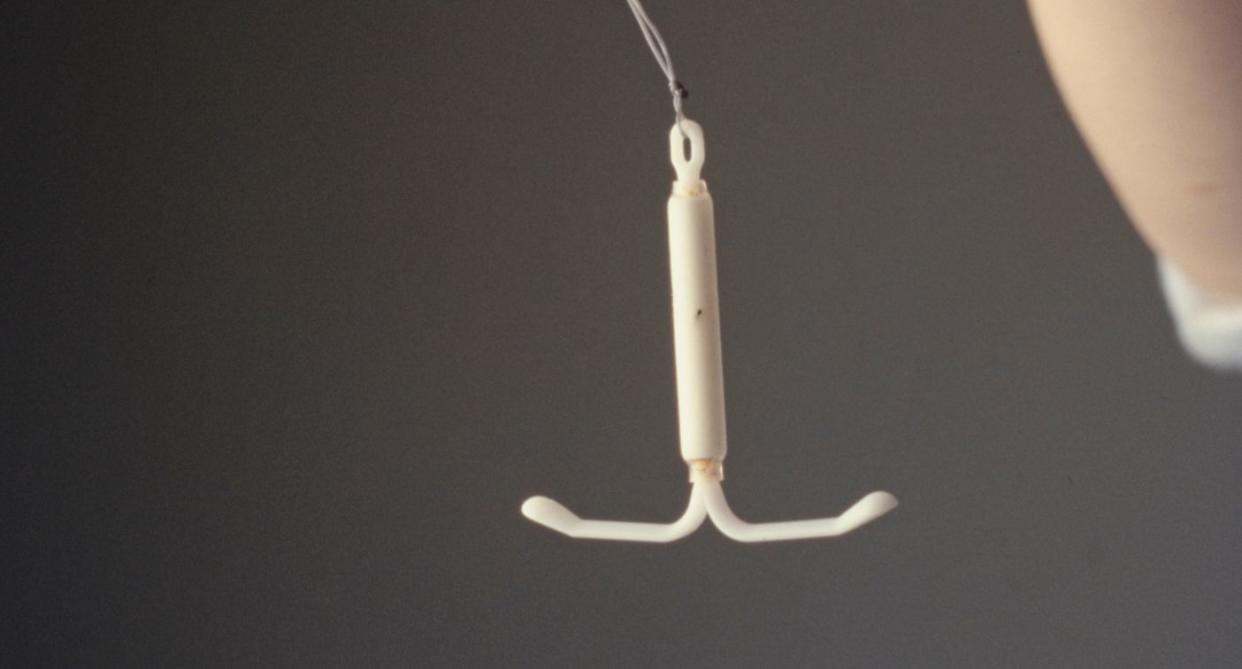
"The hormonal coil, also known as the intrauterine system (IUS), can affect your skin and potentially cause outbreaks," says Dr Paolino.
"The progestin, a synthetic form of progesterone, released by the hormonal coil can lead to changes in your body’s natural hormone levels. Hormones play a significant role in regulating sebum (oil) production in the skin, and an increase in progestin can sometimes lead to increased sebum production, which can clog pores and result in acne"
The dermatologist says this is especially the case in individuals already prone to breakouts.
"Some progestins have mild androgenic effects, meaning they can mimic male hormones like testosterone, which are known to increase oil production in the skin. This can contribute to the development of acne, particularly on the face, chest and back," Dr Paolino adds.
"Additionally, hormonal fluctuations caused by the coil can also lead to increased skin sensitivity, making your skin more reactive to other acne triggers, such as stress, diet or skincare products."
Should I remove the hormonal coil to improve acne?

"IUDs and IUSs are a highly effective and convenient form of contraception. Whether or not to remove the hormonal coil due to skin issues is a personal decision and should be made in consultation with your doctor as there may be other factors which are driving your acne breakouts," advises Dr Paolino.
"If your acne is mild and manageable with skincare or medication, it may not be necessary to remove the coil. However, if the acne is severe, persistent, or affecting your quality of life, it could be worth discussing alternative contraception methods with your doctor.
"It’s important to weigh the benefits of the hormonal coil, such as long-term birth control, lighter periods and reduced menstrual cramps, against the side effects of acne when making your decision. It’s important to note that there are also prescription medications such as spironolactone and isotretinoin which can safely be taken alongside your hormonal coil to treat acne."
What happens if you do decide to remove the hormonal coil?
How long until I see an improvement in my skin?

"If you choose to remove the hormonal coil, your body will go through a period of adjustment as hormone levels stabilise. This process can take a few weeks to several months, depending on your body’s response," Dr Paolino points out.
"Immediately after removal, you might notice a temporary increase in breakouts as your body adjusts to the absence of synthetic hormones. Over time, your natural hormone levels should begin to stabilise. For many people, skin issues caused by the hormonal coil improve within three to six months after removal.
"However, some might see improvements sooner, while others may take longer. During this adjustment period, maintaining a consistent skincare routine, avoiding harsh products, and possibly seeking advice from a dermatologist can help manage any skin issues."
What other contraception options are there?

"First, it’s important to recognise that hormonal contraceptives can have varying effects on the skin," says Dr Babak Ashrafi of Superdrug Online Doctor.
"Some options, like combined oral contraceptive pills containing both oestrogen and progestin, can actually improve acne by balancing hormone levels that contribute to breakouts. Pills that contain low-androgenic progestins, such as drospirenone (found in Yasmin or Yaz), are particularly beneficial for managing acne." Though these may come with alternative effects, of course.
"On the other hand, progestin-only pills, the implant, or injection might exacerbate acne for some people due to their androgenic effects," adds Dr Babak.
Dr Paolino says another option of course includes the non-hormonal coil (or copper coil or IUD). While this is hormone free, some may find it tougher to adjust to than the IUS, though it could be worth it in the long run.
"Each option has its own set of benefits and side effects, which should be considered based on your individual health needs," she adds.
Natural alternatives

Sick of having all this to consider, you understandably might be tempted to look at natural methods (Natural Cycles might ring a bell). But it's very important to consider the safety of this.
"Recent research has found 4% are using natural methods of contraception and two-thirds of those using this method were happy using it. However, if you're considering natural family planning, it's advisable to work with a healthcare provider who can provide guidance on the method best suited to your individual circumstances," says Dr Babak. "Additionally, couples should be aware that these methods do not protect against sexually transmitted infections (STIs), so other precautions may be necessary if STI prevention is a concern."
Dr Babak also warns that using natural family planning methods as contraception can also be risky because they require a lot of attention to become accurate. "Understanding your cycle enough to know your fertile window can take up to six months of tracking your temperature and cervical mucus, meaning the effectiveness can be influenced by user adherence to the method and the specific characteristics of an individual's menstrual cycle," he explains.
"This method is not advised for people with irregular cycles, as they are harder to track. It's important to note that natural family planning methods do not provide the same level of protection against pregnancy as hormonal contraceptives or barrier methods; however, they are side effect-free."
Consult your doctor about what is right for you.
Natural Cycles spokesperson, Lauren Hanafin, says, "While sometimes confused with traditional natural family planning methods, the Natural Cycles birth control app is a regulated medical device powered by an algorithm that not only makes it more effective than traditional FAMs by removing human error, but makes it easier to use."
Read more: Going on holiday can mess up birth control. Here's how to stay on top of it (Yahoo Life UK, 6-min read)
Read more: Why your thyroid can have such a big impact on your health (Yahoo Life UK, 6-min read)


