Scientists make discovery behind the connection between cancer and obesity
Scientists have unlocked a key piece of information that might explain the so-called “obesity paradox” for cancer patients.
The fact that obesity can contribute to cancer progression but also improve a patient’s response to immunotherapy is known as the “obesity paradox” among researchers.
Now academics, led by scientists from Vanderbilt University Medical Centre in the US, have made a discovery behind the “complicated connection” between obesity and cancer – and hope that one day it could lead to improvements in a type of cancer treatment called immunotherapy.
A new study, published in the journal Nature, outlines how immune system cells called macrophages play an unexpected role in this connection.
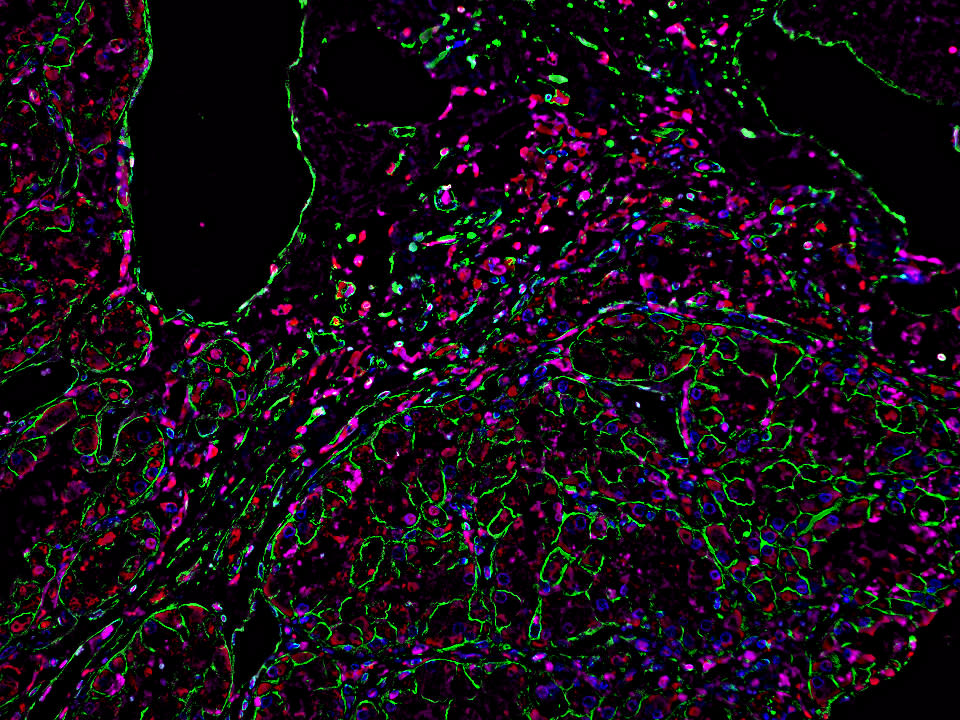
By studying mice and tumour samples from kidney cancer patients, they found that obesity increases the number of macrophages in cancer tumours and increases their production of a protein called PD 1.
PD 1 is a target of cancer immunotherapies – a type of medicine which harnesses a patient’s own immune system to fight cancer.
Researchers said that increased PD-1 suppresses “immune surveillance” by macrophages — and as a result, suppresses the killer T cells (the immune cells that can kill cancer cells) — which in turn allows tumours to grow.
This could help explain the increased cancer risk linked to obesity, they said.
Academics said that PD 1 also acted directly on the macrophages to suppress their function – so when the protein was blocked with immunotherapy, it helped these PD-1-expressing immune system cells to perform their role in the immune system.
This could explain why obese people can have a better response to immunotherapy, they added.
By studying human tumours, they also found that when people lost weight, the PD-1 expression in macrophages in tumours appeared to decrease.
Professor Jeffrey Rathmell, director of the Vanderbilt Centre for Immunobiology, said: “Obesity is the second leading modifiable risk factor for cancer, behind only smoking, and obese individuals have a greater risk for worse outcomes. But they also can respond better to immunotherapy. How is it that there can be this worse outcome on one hand, but better outcome on another?
“We clearly want to find ways to make immunotherapies work better, and in the obese setting, they naturally work better.
“Understanding how these processes are working biologically may give us clues about how to improve immunotherapy in general.”
Lead author, postdoctoral fellow Dr Jackie Bader, added: “Macrophages are thought of as being like a garbage truck: They clean up the mess. But they have a huge spectrum of activity to enhance the immune response, and they’re more plastic and manipulatable than other immune cells, which makes them really interesting.”
“We were very fortunate to have collaborators that provided us with samples from the same patients before and after weight loss that reinforced the findings from our mouse models.”
She continued: “It could be that the greater the proportion of PD-1-expressing macrophages a tumour has, the better the response to immunotherapy will be.”


